Chronic inflammation in benign prostate tissue is associated with aggressive prostate cancer, according to a study published in Cancer Epidemiology, Biomarkers, & Prevention, a journal of the American Association for Cancer Research.
An analysis of prostate tissue biopsies collected from some participants of the placebo arm of the Prostate Cancer Prevention Trial (PCPT) found that those whose benign prostate tissue had chronic inflammation had 1.78 times higher odds of having prostate cancer, and 2.24 times higher odds of having an aggressive disease (characterized by Gleason sum of seven to 10), compared with those whose benign prostate tissue had no inflammation.
“We had the unique opportunity to investigate biopsy tissue from patients who had no indication to prompt a biopsy,” said Elizabeth A. Platz, Sc.D., MPH, professor in the Department of Epidemiology at the Johns Hopkins Bloomberg School of Public Health and member of the Sidney Kimmel Comprehensive Cancer Center in Baltimore, Md. “Participants in the PCPT who were not diagnosed with prostate cancer during the trial were recommended to undergo prostate biopsy at the end of that trial, which meant that prostate tissue was available not just for men who had the diagnosis of prostate cancer, but also for those who did not have the diagnosis.
“We found that men who had at least one biopsy core with inflammation had a higher likelihood of having high-grade prostate cancer compared with those who did not have any inflammation in their biopsy tissue,” said Platz. “While we know that inflammation is common in prostate tissue from men who have some indication to prompt a biopsy, such as high PSA or an abnormal digital rectal examination [DRE], we were surprised to find that the prevalence of chronic inflammation in the men who didn’t have any such indication was really high, about 78 percent.”
Between 1993 and 1997, 18,882 men who were at least 55 years old and had a normal DRE with a serum PSA of 3 ng/ml or less, were recruited to the PCPT. All participants completed questionnaires that included demographics, lifestyle, and medical factors, and were followed for seven years after they were randomly assigned to receive either finasteride or placebo.
The investigators screened all participants for prostate cancer by PSA and DRE during annual visits. Those who had an indication underwent a “for-cause” biopsy if they had cancer, and those who did not have prostate cancer diagnosed during the trial were recommended to undergo an “end-of-study” biopsy at the end of the trial even if they did not have an indication.
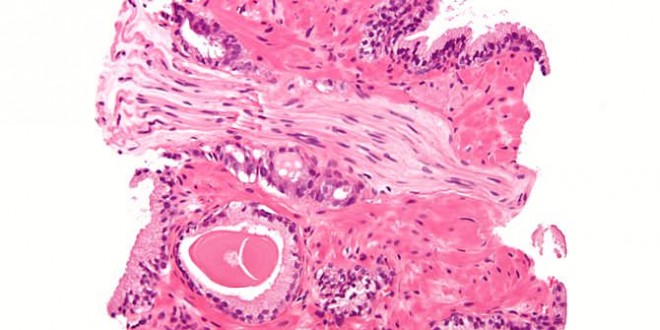
From the placebo arm of this study, Platz and colleagues sampled 191 prostate cancer cases and 209 frequency-matched controls for whom biopsy tissue was available. They performed histopathological evaluation of the biopsy samples to identify the prevalence and extent of inflammation, and types of inflammation, i.e., acute or chronic inflammation.
They found that 86.2 percent of cases and 78.2 percent of controls had at least one biopsy core with inflammation, most of which was chronic, and this difference was statistically significant. They also found that the association between chronic inflammation and aggressive prostate cancer did not change after adjusting for known risk factors including body-mass index, pack-years of cigarettes smoked, and history of diabetes.
In addition, this association held true even among men whose PSA levels were less than 2 ng/ml. “We detected chronic inflammation in prostate tissue of men who had prostate cancer but had PSA levels lower than 2 ng/ml, and thus our work supports an association between inflammation and prostate cancer that is not explained by PSA-associated detection bias,” said Platz.
Among men whose PSA levels were less than 2 ng/ml at the time of biopsy, those whose prostate tissue had inflammation had 4.11 times higher odds of having aggressive prostate cancer, compared with those whose prostate tissue did not have any inflammation.
“Our team is next studying the type of inflammatory cells that may be influencing the risk of aggressive prostate cancer,” said Platz. “This study is a stellar example of multidisciplinary research involving epidemiologists, pathologists, immunologists, urologists, and biostatisticians,” Platz added.
Angelo De Marzo, M.D., Ph.D., professor in the Department of Pathology at the Johns Hopkins Hospital, is a co-leader of this study.
This study and the PCPT, which was conducted by Southwest Oncology Group, were funded by the National Cancer Institute. Platz and De Marzo declare no conflicts of interest.
Canadajournal/Press Releases
 Canada Journal – News of the World Articles and videos to bring you the biggest Canadian news stories from across the country every day
Canada Journal – News of the World Articles and videos to bring you the biggest Canadian news stories from across the country every day