A new type of implantable device may curb central sleep apnoea in patients with heart failure, indicate the results of a one year pilot study* presented today at the World Congress on Acute Heart Failure in Athens.
Central sleep apnoea occurs in around a third of heart failure patients and doubles their risk of death. But the condition has proved difficult to treat successfully.
CSA is a comorbidity in more than a third (35 per cent) of heart failure patients approximately and doubles their risk of death. Previously, there has been no proven treatment but the new remede system uses unilateral transvenous phrenic nerve stimulation to prevent CSA before it occurs.
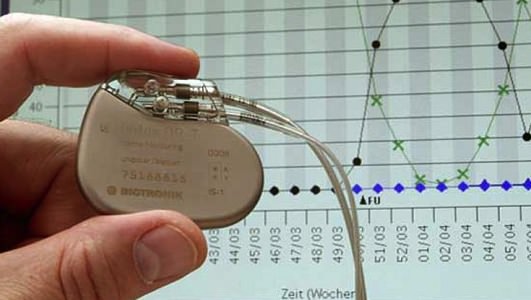
Working similarly to a pacemaker, the device is placed under the skin and connected to the veins near the phrenic nerve.
Professor William T. Abraham from Ohio State University, who led the study, said the remede system gave patients more energy and the ability to do their normal daily activities without falling asleep.
He said: “The device stimulates the diaphragm via the phrenic nerve, causing the diaphragm to contract. It regularises the patient’s breathing pattern throughout the night, rather than waiting until the patient stops breathing to react.”
Some 46 patients were included in the study, all diagnosed with moderate to severe CSA and implanted with the remede system. The pilot study, multicentre trial, found a reduction in apnoea hypopnea index (AHI) at three months compared to baseline with six- and 12-month data also collected.
The one-year results show that the remede system has had substantial benefits for the patients concerning their quality of sleep, including a reduction in AHI, a reduction in the time spent with low blood oxygen levels overnight, and improvements in sleep efficiency and REM sleep.
According to the study, the device also improved important cardiac endpoints such as heart rate variability, which is a measure of autonomic balance. It also found there were other changes to the structure and function of the heart, called reversed remodelling. Patients with the implantable device noted a smaller heart, making the left ventricular diastolic volume significantly smaller and the heart became stronger.
These, according to Professor Abraham, are changes that “generally correlate” with improvement in long-term clinical outcomes.
Agencies/Canadajournal
 Canada Journal – News of the World Articles and videos to bring you the biggest Canadian news stories from across the country every day
Canada Journal – News of the World Articles and videos to bring you the biggest Canadian news stories from across the country every day