People are more at risk of schizophrenia if they inherit genes that lead to excessive loss of healthy brain synapses during adolescence, a major US study suggests.
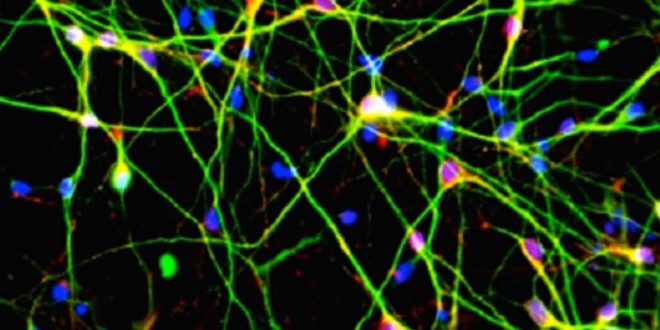
Schizophrenia is known to have a genetic component but the research, published online in Nature on Wednesday, links the disease with specific gene variants and a biological process called synaptic pruning – the elimination of connections between neurons, or brain cells.
The link between schizophrenia and a protein called complement component 4, or C4, was painstakingly established by combining a genetic screen of more than 65,000 people with laboratory findings in mice and analysis of 700 postmortem brain samples. Researchers said they believe the protein plays a role in signaling which connections between neurons should be “pruned,” or removed, as the brain develops after childhood.
“This suggests one possible model for schizophrenia that makes sense of a series of observations about the disease that previously seemed disconnected,” says Steven A. McCarroll, director of genetics at the Broad Institute’s Stanley Center for Psychiatric Research and the senior author on the paper, which was published today by Nature.
Scientists have long puzzled over why schizophrenia strikes in late adolescence or early adulthood, sending previously high-functioning individuals spinning into psychosis and often leaving them with devastating cognitive deficits. Although the cause of schizophrenia is unknown, a growing body of evidence has shown its onset is usually accompanied by the massive loss of synapses, the microscopic connections between brain cells.
Tyrone Cannon, a professor of psychology and psychiatry at Yale University who studies schizophrenia and was not involved in the research, called the paper “a big step forward” because “it helps to link up findings from the genetics of schizophrenia, which are highly complex, to findings on what the underlying neural problems of schizophrenia might be.”
The work began four years ago, inspired by papers that three consortia from around the globe published in 2009. These compared DNA differences between the genomes of people with schizophrenia and the genomes of people without the disease. All three analyses pointed to a swath of genetic real estate consisting of hundreds of genes located on the short arm of chromosome 6 and associated with the immune system. At first, geneticists were unable to discern any real pattern in the data. Part of the reason, McCarroll says, was that there were not one or two DNA differences that on their own seemed to be consistently associated with an increased risk for the disease.
After eliminating all conventional explanations, McCarroll says, his graduate student Aswin Sekar eventually identified a possible pattern: many of the DNA variations seemed to affect the amount of a specific type of C4 protein present in the synapses of the brain. And the more C4 was present, the higher the risk of developing schizophrenia. “There are many forms of C4, each with a different level of risk, and that underlying complexity was what had made this appear to be such a hard problem scientifically,” McCarroll says.
McCarroll says that certain versions of the C4 gene seem to increase people’s risk for developing schizophrenia by 27 to 50 percent.
But what is the biological role of C4 in the brain? The gene clue would have been wholly perplexing, McCarroll says, were it not for groundbreaking 2007 work by Beth Stevens, who today runs a laboratory at Boston’s Children’s Hospital. The C4 gene participates in what’s known as “the complement cascade,” a process by which the immune system marks tumors, viruses, or dying human cells for elimination and removal. What Stevens, along with Stanford biologist Ben Barres, found was that the complement cascade also plays a novel role in brain development early in life. Specifically, the system helps to “prune” unneeded or unused synaptic connections, sculpting the brain into a more efficient structure. Stevens demonstrated that complement molecules were serving as an “eat me” signal, summoning tiny cells in the brain known as microglia to converge on unused synapses and prune them away.
After Sekar and McCarroll traced the schizophrenia mutations to C4, they got in touch with Stevens, whose lab is devoted to studying microglia, and the two labs began to hold joint weekly meetings. Working with mouse models, they soon demonstrated that C4 also had a role in synaptic pruning in the brains of developing mice. Their theory now is that excessive levels of the protein could lead to overpruning and to the thinning out of brain tissue that appears to coincide with the worsening of schizophrenia symptoms, such as psychotic episodes. Cannon says psychosis is likely caused by tissue loss in regions of the prefrontal cortex that help individuals establish information flow and identify whether stimuli they are experiencing come from the outside world or from within their own head.
Cannon says the new study is important for having taken a clue from a genetic screen, added evidence from animals, and then related the data to what’s known about schizophrenic patients. “Schizophrenia is one of those conditions that defy explanation with respect to any one gene,” he says. The new result, however, suggests ways to “integrate” what happens in different brain regions, pathways, and transmitter systems. “It seems compatible with the general view that many different kinds of mutations will aggregate together to drive somebody toward a threshold effect that could result in overly aggressive immune signaling and gray-matter loss,” he says.
Steven E. Hyman, director of the Stanley Center for Psychiatric Research and a former director of the U.S. National Institute of Mental Health, called the paper “a landmark” and noted that “it begins to suggest potential routes toward therapies.” New drugs are urgently needed. Schizophrenia is currently treated with antipsychotic medications that help stop hallucinations but don’t do much for the other symptoms, including poor decision making and memory problems.
Agencies/Canadajournal/Press Releases
 Canada Journal – News of the World Articles and videos to bring you the biggest Canadian news stories from across the country every day
Canada Journal – News of the World Articles and videos to bring you the biggest Canadian news stories from across the country every day